Blog 2: Substance Use, Addiction and the Opioid Epidemic
Examining the historical legacy of opioids on America provides several key insights into the current opioid epidemic:
· Medical use and overprescribing. Historically, opioids were believed to be safe for patients and non-addictive. Marking and promotion of the medication made it readily available and socially acceptable.
· Pharmaceutical influence and marking campaigns that were misleading consumers.
· Stigmatization around substance abuse disorder. This has shaped communities and societies into how they view people struggling with substance use.
· Policy response, focused on punitive measures rather than treatment focused approaches (Quinones, 2021).
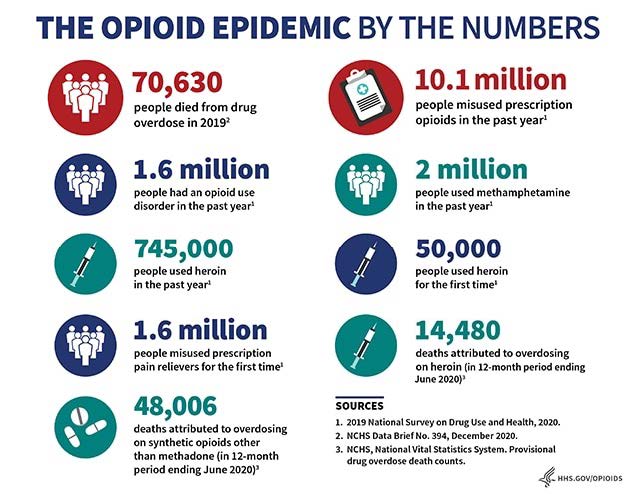
https://www.hhs.gov/opioids/statistics/index.html
Substance abuse in America
o Incarceration rate much higher than the rest of the world
o Roughly about 11% of Americans with opioid use disorder receive treatment (Coulson, 2023).
1. Barrier to seeking help: Patients can fear being labeled or judged preventing them from seeking proper treatment.
2. Limits access to resources: stigmatization can affect funding and support for treatment programs.
3. Internalized Stigma: Patients that struggle with substance use can internalize negative stereotypes which can lead them to feel shame.
4. Quality of care and poor patient outcome: stigmatization can impact how healthcare providers interact with patients. Discrimination or bias can lead to inadequate care (Amarendran, 2024).
Treatment for Substance use disorder
1. Assessing and screening patients: Performing a thorough assessment of the patient to understand the substance use history, medical and psychological condition, and if there are any other co-occurring disorders.
2. Treatment plan: Together with the patient come up with a personalized plan that outlines patient’s goals.
3. Withdrawal management: Inpatient and medical supervision might be necessary for safe withdrawal.
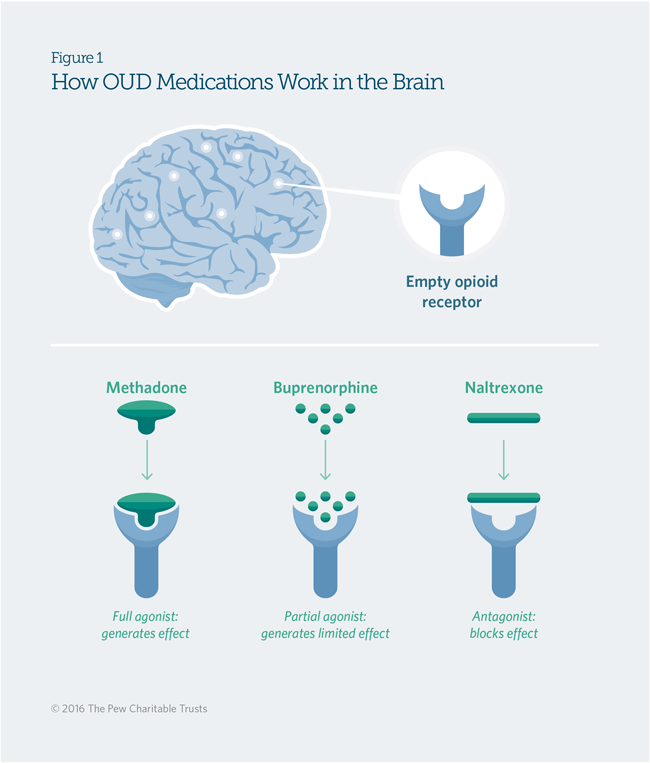
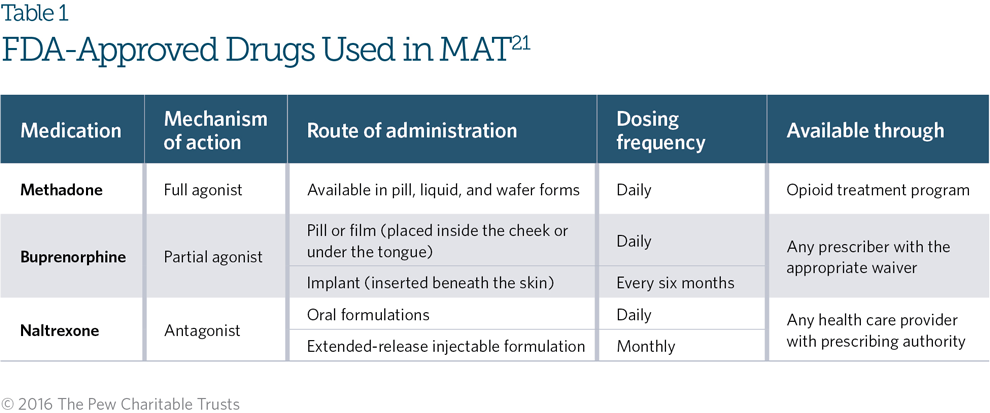
4. Medication Assistant treatment: Medications should be considered to help with cravings and withdrawal symptoms. For opioids the following medications can be considered Suboxone, Methadone, and Naltrexone.
5. Psychosocial Interventions:
1. Evidence-based therapies
2. Community resources for support
6. Ongoing monitoring and follow up: Building a therapeutic relationship with the patient will enhance the effectiveness of treatment process.
In conclusion, the interview that Dr. Eldershaw conducted with Andrew was eye opening. The importance of having a well-structured program and medical help that Andrew received during his treatment for substance use disorder was significant. This approach to treatment made a difference for him and helped him stay substance-free. He talked about how significant it was for him for having medication assistant therapy with the program and this stood out to me especially as a future prescribing health care provider.
References
Amarendran, V. (2024, October). Stigma in substance use disorder treatment. Lecture.
Coulson, M. (2023). Barriers to methadone access. Johns Hopkins Bloomberg School of Public Health. https://publichealth.jhu.edu/2023/barriers-to-methadone-access
Quinones, S. (2021). The least of US: True tales of america and hope in the time of Fentanyl and meth. Bloomsbury Publishing.
Comments
Post a Comment